A mysterious disease swept the world in the early 1920s that put people into catatonic states; stiff and immovable like human statues. It was called encephalitis lethargica and it affected over 5 million people worldwide, and then was almost forgotten.
TRANSCRIPT:
In 1969, Beth Abraham Hospital in New York had a patient named Leonard. Leonard had not left the hospital in thirty years.
He was one of a group of patients who had been there since before some of the nurses were even born. They all suffered from a mysterious illness that swept the country in the early 20th century, one that left them in a catatonic state, frozen inside their own bodies, like human statues.
Nobody knew what was going on inside there. Were they conscious? Unconscious? Something in-between? Or worst of all, were they wide awake, fully aware of what was going on around them, and just unable to get their brains to talk to their bodies? Nobody knew.
Then, in March of 1969, Leonard and the others were going through their daily routines; food, cleaning, medicine, when the doctor came in and gave each of them an oral medicine to drink.
There was nothing unusual about this, they were always tweaking their medicines and the doctors were always testing out new drugs that might help their condition. The nurses didn’t even ask what it was, it was so routine.
After Leonard got his medicine, they wheeled him into the rec room, where the other patients were sat around TVs and stereos and whatnot, and after staring blankly at the TV screen for a half hour or so, Leonard… Woke up.
And started to talk.
Where had he been this whole time? What was this sleeping sickness that put him in that state and what was the drug that got him out?
And the most important question… Could it happen again?
I’ve talked in multiple videos at this point about the beginning of the 20th century and how quickly things were changing and evolving. It comes up a lot actually. In fact… I think I talked about it last week…
But it really was a crazy time, just think about how many things happened in just a couple of decades. People’s homes got gas lines, then indoor plumbing, then electricity. Radio became a thing, then movies, cars were invented, then airplanes. World War 1 brought untold devastation and killed 20 million people, then the Spanish Flu swept the world and killed 50 million more.
Just to put that into perspective, the global population was around 1.6 billion at the turn of the century. Between World War 1 and the Spanish Flu, nearly 5% of the world population was wiped away.
So, if you knew more than 20 people, you knew someone who died from one of those two things.
But just as things were settling down and the world began to recover and prepare for a Great Depression and even bigger World War 2, somewhere in the middle of all of that came one of the most bizarre and still unexplained global pandemics of all time.
By the way, I should point out that I covered this topic in an episode of my Mysteries of the Human Body series over on Nebula. I’ll go way more in-depth about it here but it was an episode on mysterious plagues so if you want to see more stories like this, you can find some there.
It all started in the winter of 1916 in Europe, when patients began showing up in hospitals complaining of an extreme malaise, a total lack of energy and an overwhelming desire to sleep.
Some showed other neurological symptoms as well like tremors and palsies and hyperkinetic movements.
And in extreme cases, the patients were in basically a comatose, catatonic state, unable to move or react to their environment.
Luckily for most people, the disease ran its course and they went on with their lives, though there was ongoing neurological damage as we’ll talk about later.
But for some, this became their permanent existence. And more of these cases seemed to pop up every day.
The disease got the attention of a doctor from the Psychiatric-Neurological Clinic of the University of Vienna, who had examined a handful of patients with this disease, and he was the first doctor to write a paper about it.
His name was Dr. Constantin von Economo, which unbelievably isn’t the name of a Marvel villain with the power to destroy the economy.
He wrote about it in a paper published in the journal Wiener Klinische Wochenschrift in 1917.
That’s the Vienna Clinical Weekly to you non-Germans out there.
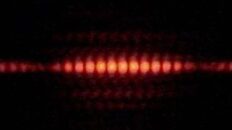
In this paper, he gave the disease a name, encephalitis lethargica. Often shortened to just E.L. Also known as sleeping sickness.
He broke down several different types of the disease, because all patients present a little bit differently, and because he was the first to publish, his name kinda stuck. In fact, it’s sometimes referred to as Von Economo disease.
He wasn’t the last person to publish on this disease, though, not by a long shot. The French physician René Cruchet was treating patients at a military psychiatric facility and published descriptions of the disease very soon after Von Economo.
Overall, there would be around 9,000 papers published about E.L. by the mid-1920s.
British epidemiologist F.G. Crookshank published a paper in 1918 that listed several other epidemics that looked like E.L. in the past.
Like, Germany’s Kriebelkrankheit in 1672-75, Rafania in Sweden in 1754-57, and the Sweating Sickness in England in 1485.
E.L. made its way to North America when the first case showed up in New York City on Sept. 4, 1918.
Within a month, three other cases were reported.
E.L. spread quickly in the U.S. during the last half of 1918, and by the spring of the next year, it had been reported in 20 states.
The disease peaked worldwide in 1923 when 2,000 people in the U.S. died from it. And literally millions around the world were infected with it.
It’s about as close as you can imagine to a real live zombie outbreak. Hundreds of thousands of people lost the ability to walk, talk, and function, spreading further and further with nothing short of world domination in sight.
And then, around 1925, it just kinda… stopped. New cases stopped popping up, except for a few here and there. Those that had it eventually overcame the disease and went on with their lives, and the whole affair was mostly forgotten.
Over the decades, doctors studied these surviving patients looking for clues to the disease’s origin and pathology. And while most of it remains a mystery, some patterns did emerge.
Dr. von Economo classified E.L. into three forms: amyostatic-akinetic, hyperkinetic, and somnolent-ophthalmoplegic.
The least common of the three is amyostatic-akinetic.
In these cases, people experienced rigidity for extended periods. But they are aware of what’s happening, just their movements are very slow.
As Dr. von Economo wrote:
The hyperkinetic form presented with a manic phase at the beginning with involuntary, jerky movements in their faces, hips, and shoulders, and some vocalizations.
That’s just the first phase, after that they experience fatigue, restlessness, and weakness, which can last for several days. During this phase some people experience hallucinations and nerve pain in their faces and limbs.
But the most common form was the somnolent-ophthalmoplegic type of E.L. Its characteristics include confusion, delirium, and feelings of being in a dazed state.
Other signs are cranial nerve paralysis and an overwhelming desire to sleep.
And of the people who die from it, about a third of them die from respiratory failure.
Parkinsonism
One interesting link that did get made was between E.L. and Parkinsonism, which a lot of patients developed after the epidemic faded away.
By the way, Parkinsonism is a catch-all term for any neurological condition that causes stiffness, tremors, and slowed movements.
So yeah a lot of these E.L patients would recover, but then later develop this kind of Parkinsonism where they’d become mentally and physically exhausted, their limbs would become rigid, their postures bent, and their walking unsteady. This would all happen over a few months.
This isn’t the same as, say, Parkinson’s Disease – that presents way differently so doctors started to call it postencephalitic Parkinsonism, or PEP.
Some of the differences between the two include:
- PEP occurs at any age; Parkinson’s occurs generally after age 50
- PEP progresses rapidly and in spurts; Parkinson’s steadily progresses
- No sign of “pill-rolling” tremors in PEP, which you often see in Parkinson’s.
Pill-rolling tremors are movements that look like you’re rolling a pill between your index finger and thumb.
Look out, Matthew Mcconaughey.
The majority of cases showed up during the 1920s about six months to a year following acute E.L. Some studies suggest that the number of patients with Parkinsonian symptoms tripled during that time.
Since there were so many PEP cases in the 1920s and 30s, many doctors believed E.L. caused Parkinsonism.
They even thought that Parkinsonism would disappear when the E. L. generation died out.
Would have been nice, but that’s not what happened.
Oliver Sacks
And many of them did die out over the years, many from complications from E.L., many from the Parkinsonism. But some just kept on going, trapped in their faulty bodies, year after year, with no answer in sight.
Jump ahead to the 1960s where our story began, where a small group of these survivors resided at the chronic-care facility in Beth Abraham Hospital in New York.
By the way just a reminder of the timeline here, these patients had come down with this in the 20s. It was now the 1960s. So yeah, four decades had passed.
Then in 1966, a new doctor came to work with these patients, a neurologist named Dr. Oliver Sacks.
He had just completed a residency in neuropathology at UCLA and was interested in exploring this and other neurological “edge cases” that he’d read about.
When he first arrived on the ward, he described it as like entering a museum or waxwork gallery.
As he would later write in his book:
“They would be conscious and aware – yet not fully awake; they would sit motionless and speechless all day in their chairs, totally lacking energy, impetus, initiative, motive, appetite, affect or desire; they registered what went on about them without active attention, and with profound indifference. They neither conveyed nor felt the feeling of life; they were as insubstantial as ghosts and as passive as zombies.”
He said they were motionless people fixed in strange positions, and everything looked frozen.
And that was a characteristic of these patients, like if you raised a person’s arm in the air, they would hold it there until you moved it back down. People basically acted like posable figures. They really were human statues.
Then in early 1967, a new treatment became available to treat Parkinson’s disease, called Levodopa, or L-dopa.
It works by increasing the body’s ability to produce the hormone dopamine, which makes it possible for your brain to effectively transmit signals down neural pathways. And that’s one of the root causes of Parkinson’s disease, your body stops being able to produce dopamine, and it screws up the communication signals in the brain’s motor cortex.
L-dopa is a precursor to dopamine. It’s a chemical your body needs to make the dopamine, so by giving Parkinson’s sufferers L-dopa, it helps them make dopamine and that slows the progression of Parkinson’s symptoms.
Sacks described it as kind of like a nutrient that serves to replace missing dopamine. It’s dopamine fertilizer, if you will.
And since there’s a documented connection between E.L. and Parkinson’s, he started to wonder if it would work on E.L. patients, too.
It took a couple of years to get access to L-dopa and get permission but finally in March 1969 he was able to administer L-dopa to them. And it worked. The patients awakened and acted normally.
These patients who had been catatonic or straight-up asleep for forty years suddenly came to life. They were conscious, they were coherent, they were able to move and walk and play, throw balls to each other. It was like a literal miracle.
Some were excited to be back to their normal lives, but some others couldn’t handle the sudden transformation and acted violently or regressed back into their “sleepiness.”
As he told Fresh Air in 1985:
I mean, think about it, when they went into that state, Charles Lindbergh hadn’t flown across the Atlantic yet. And just months after they woke up, we landed on the moon.
Many of them would look in the mirror and were confused by the old person staring back at them. And of course the music and the fashion were bizarre and confusing to them.
Have I been asleep for decades?
Unfortunately, after several months of being awake and experiencing life, the L-dopa started to wear off. Each dose produced diminishing returns and eventually, they stopped responding to it altogether and returned to their catatonic state.
Sacks wrote about the experience in his book Awakenings, which of course was turned into an Oscar-winning movie starring Robert De Niro and Robin Williams.
What Causes E.L.
Next year will mark 100 years since the end of the encephalitis lethargica epidemic. And we still have no clear idea of what caused it. But there are some theories.
Traditionally, theories have fallen into two main categories: toxicological and infectious. A third one has popped up in more recent years but I’ll get to that one in a minute.
Toxicological obviously means caused by an external toxin of some kind. For example, at one time in England, it was thought to be botulism or solanine that can collect in potato sprouts.
Dr. von Economo ruled out toxic causes like food poisoning early on because they didn’t have any gastrointestinal issues.
He also ruled out typhoid, polio, syphilis, and poison gas.
But what he did notice was that all of the patients had influenza-like symptoms. Since they were still coming out of the Great Influenza pandemic, he thought maybe was an encephalitis related to the flu.
And there were previous instances of E.L. associated with flu epidemics.
Unfortunately, studies showed that the brains of people who died from an influenza encephalitis had significant neuropathological differences than people who died from E.L. But still, Dr. von Economo believed that an infectious virus caused E.L.
There have been various studies over the years that both support or deny the influenza-cause theory. So it’s never fully been proven, but it would explain why the disease suddenly went away about the same time as the influenza pandemic ended.
But I did mention a third hypothesis earlier. That one was proposed in the early 2000s and it suggests it was caused by a post-infectious autoimmune disorder.
For specifically the hyperkinetic form, researchers proposed antibodies against NMDA receptors could cause E.L.
Without getting too in the weeds, NMDA is a receptor for the neurotransmitter glutamate, it stands for N-methyl-D-aspartate, and it helps with neuroplasticity.
So the idea is that the body is creating antibodies that are attacking the NMDA receptors, which kinda short-circuit the brain.
This hypothesis was put forth by Russell Dale, a pediatric neurologist working in the U.K. in 2003.
He was actually working with some E.L. patients, which by the way, plot twist, there are still cases of this popping up here and there.
But he was working with around 20 patients when he noticed that more than half of them had experienced a sore throat caused by a rare form of strep just before they started suffering from E.L.
Tests showed that NMDA antibodies were elevated in those patients. He hypothesized that the antibodies may have mistakenly attacked the basal ganglia neurons.
But studies during the original epidemic showed abnormalities in other parts of the brain, like the cerebral cortex.
Later, in 2012, a study proposed that E.L. could be caused by an enterovirus, maybe even the poliovirus.
Enteroviruses are made of RNA and protein. They can enter the body through the gastrointestinal tract before attacking the nervous system. They can also spread through the air and on contaminated surfaces.
Anyway, the 2012 study found virus-like particles “in the cytoplasm and nuclei of midbrain neurons in all classical E.L. cases studied.”
They also found larger virus-like particles in modern E.L. cases. It should be noted that none of them were influenza particles.
While it was a well-conducted study, hasn’t been replicated.
And that basically gets us caught up to today. Again, with lots of theories, and not a whole lot of answers.
It might be easy to dismiss encephalitis lethargica as a random medical mystery from the past, but I think that doing that would be a mistake. After all, as I just pointed out, it’s not totally gone, there are still cases that crop up from time to time. Just not in the epidemic numbers we saw 100 years ago.
Although… that might not be true anymore.
Perhaps you noticed we’ve had a bit of a global pandemic ourselves in the last few years, and we’re finding an alarming trend of post-pandemic symptoms that are eerily similar to the E.L. epidemic.
In fact, that little story I told you about _, he’s not a survivor of the Spanish Flu pandemic 100 years ago. He’s a covid survivor, currently dealing with an extreme case of Long Covid.
A Long Covid Connection?
According to the CDC, 6 percent of the US adult population is experiencing long covid symptoms. That’s actually down from previous years, which is a good thing, but that’s still nearly 20 million people.
Long covid symptoms can range from lingering loss of smell and taste to extreme fatigue and mental fog. According to a recent study, 26.4 percent of covid long-haulers report significant complications in their ability to perform daily activities.
Now I should say right up front, long covid is not the same as E.L. There’s no unresponsive human statues this time around and the symptoms are a lot more nebulous. In fact, The Lancet published a paper in 2021 that found more than 200 symptoms across 10 organ systems in people who experience long COVID.
Some research suggests that microclots that form around inflammatory molecules obstruct oxygen flow into cells.
That’s why some long COVID patients feel tired, have brain fog, or can’t breathe well.
Another theory is that COVID-19 may disrupt mitochondrial function, which also makes someone feel tired or have brain fog.
But there are parallels to draw here, not just because it’s a lingering disease that was spurred on by a pandemic, but because some of those nebulous symptoms are neurological. And it’s important to get to the bottom of how viral infections can effect the nervous system, even years after the epidemic peaks.
Or as Dr. Hadi Manji of the UK National Hospital for Neurology said:
It’s going to take a long time to fully understand the ripples that the Covid pandemic put into the world. It’s kind-of impossible to see from where we’re standing at this place in history.
In fact, if the sleeping sickness teaches us anything, it’s that some of the downstream effects never fully get figured out.
Out of the tens of millions of people infected by the Spanish Flu, a small percentage developed E.L. Of those, a tiny percentage never fully recovered. It’s possible that the same could be true with long covid. And 40 years from now a small number of long covid sufferers are still bedridden, hoping for a miraculous cure.
But my god, let’s hope not.
For anybody out there who’s dealing with long covid symptoms, my heart goes out to you, I wish you the best, and know that long covid is not the same as E.L. so don’t let this video freak you out too much. Totally different things.
Researching this video has also made me wonder if there’s a connection with chronic fatigue syndrome? Something else that’s been around that induces extreme tiredness in people for long periods. I couldn’t find anything but I wonder if there’s something there.



Add comment